
Henry Dunlop, of Flourtown, Pennsylvania, does not believe in slowing down. At 73, Henry — known to all as Hank — is the president of an international agriculture company and keeps extremely active in his spare time. If he’s not working, you’ll probably find him biking, hitting the golf course, or indulging in one of many racquet sports he enjoys—tennis, pickleball, paddleball, and even padel. His commitment to physical activity is even more impressive when you consider that he was battling intense back and leg pain for more than 10 years. But thanks to Dr. Paul Park and the team at Och Spine at NewYork-Presbyterian/Weill Cornell Medical Center, Hank is now pain free and more active than ever.
“I first started experiencing intense back pain in 2012,” Hank says. “I had my first spine surgery, a discectomy, where they removed a portion of a disk in my spine. It relieved the intense pain I had, but it was just the beginning of the pain that was to come. I’d experienced a sore back and back pain, but pain going down your leg is a different feeling. I’d been feeling this way for 10 years, and it’s been a negative to my quality of life.”
Naturally, Hank sought answers. He consulted with experts and tried to get as much information as he could.
“Over the past decade, I’d seen a couple of back doctors and orthopedists,” he says. “In 2022, the pain got a little more intense, severe, and consistent. At the time, I lived on the Upper East Side. I was a patient at a geriatric group practice at Weill Cornell, which led me to see two terrific doctors at the Weill Cornell Spine Center: Dr. Michelle Chi and Dr. Ricky Singh. They performed nerve blocks – injections that temporarily blocked my nerves’ pain transmissions. It helped my cervical vertebrae, but after several attempts, it was clear it wasn’t going to be a long-term solution to my lower back. That’s when they referred me to Dr. Park to consider surgery.”
“Hank’s not alone in suffering from leg pain starting from the lower back,” says Dr. Park. “In fact, it’s a very common reason people go to their doctor. The source, however, can be multifactorial, which is why we take a multidisciplinary approach here at the Spine Center. My colleagues worked together to narrow down the source to nerve impingement in the lumbar spine — we can use advanced imaging, injection, and nerve conduction studies. Surgery is a last resort after all non-operative options are exhausted. Many patients improve without surgery and don’t end up needing me. For Hank, however, the more conservative options hadn’t worked, so we made a surgical plan to address his leg pain — to give him back his quality of life.”
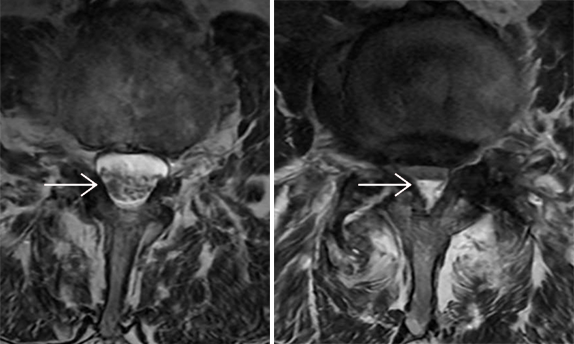
Hank Dunlop's MRI scan shows the extent of the problem. In a healthy area of his back (white arrow, left photo) the spinal cord is a normal shape. At the L3-4 level (in his lower back), the cord is severely compressed, which was causing Hank's pain.
“I found Dr. Park to be very calming,” Hank says. “He generated a sense of confidence and seemed to grasp the situation quickly. The interplay between patient and doctor is always very curious; the patient should be responsible for himself, but he relies on the doctor. So for whatever lay ahead, Dr. Park believed that surgery had a good chance of success. Ultimately, I trusted his judgment.”
With a surgery date scheduled in December, Hank took some time to reflect on how he had coped with pain over the past decade.
“Pain is a very insidious thing,” he says. “In some ways you just grow used to it — it becomes a part of your life. You can’t quantify how it affects you. There were times I’d have minimal pain and other times where I’d be pain-free. That’s the scary part. When it wasn’t hurting, I’d convince myself I was healing, that my body had found a way to adjust and be pain-free. As an optimist, I’d believe that the resolution was around the corner.” But the pain always came back.
The resolution was at hand as he walked into NewYork-Presbyterian/Weill Cornell Medical Center on a cold December day for the surgery.
“After other surgeries, my recovery tended to be a slow process. This time turned out to be borderline miraculous."
“Lumbar decompression is one of the more routine procedures we perform, however for the patient it is never routine — I believe that providing the patient with as much information as possible on the pathology and procedure is crucial, over multiple visits if needed,” says Dr. Park. “In this case the objective was to address the root cause of his leg pain. That leg pain occurs when the lumbar nerve roots are being irritated — this can be from a disc herniation, from bony arthritis, or a thickened ligament around the spinal canal. A lumbar decompression is an excellent procedure to relieve this pressure without disrupting the surrounding structures.”
The surgery was successful, and Hank was released from the hospital the same day and ready to recover at home. Having had surgery before, he thought he knew what he was in for.

Paul Park, MD, MMS
“After other surgeries, my recovery tended to be a slow process,” says Hank. “This time turned out to be borderline miraculous. After this surgery, I approached activity gradually and cautiously. I would typically wake up with pretty intense pain, improve midday, and by the end of the day my body would be exhausted and stressed out. Then, at around three weeks post-op, I woke up feeling a bit better. The following day was better yet. And within 72 hours of that I was virtually pain-free.”
Hank’s back pain is now behind him. He’s back to his active life, racquet in hand, and when we caught up with him he was about to jet off to Denmark and Sweden. “My quality of life has definitely improved,” he says. “It’s markedly better. What works for one person is not going to apply to everyone, but if there’s anyone going through the same thing, I say reach out to experts and get as much information as you can. Listen to the experts!”